Community Support Workers, Non Profit Foundation
Mammograms and Bone Density exams during breast cancer
My Digital Publication
By Nelfa Chevalier

Mammograms
A mammogram is an X-ray image of the breast utilized to detect early signs of breast cancer, often before symptoms manifest. Regular mammography screening has been shown to reduce breast cancer mortality by enabling early detection and treatment. The U.S. Preventive Services Task Force recommends that women aged 40 to 74 at average risk undergo mammograms every two years.
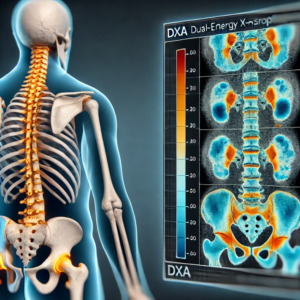
Bone Density Exams
Bone density exams, or dual-energy X-ray absorptiometry (DXA) scans, measure bone mineral density to assess osteoporosis risk. While not directly used for breast cancer detection, these exams are significant for breast cancer patients, especially those undergoing treatments that may affect bone health. Some studies have explored the relationship between bone mineral density and breast cancer risk, suggesting that higher bone density might be associated with an increased risk of breast cancer.
The connection between mammography and bone density in relation to breast cancer lies in their role in early detection, risk assessment, and managing the effects of breast cancer treatments. Here’s how they are interconnected:
- Mammography and Breast Cancer Detection
- Primary Screening Tool: Mammograms are the most effective imaging test for the early detection of breast cancer. They help identify tumors before symptoms appear, improving survival rates.
- Breast Density Impact: Women with dense breast tissue have a higher risk of breast cancer and may require additional imaging, such as MRI or ultrasound, to enhance detection accuracy.
- Bone Density and Breast Cancer Risk
- Bone Mineral Density (BMD) as a Risk Factor: Some studies suggest that higher bone density is associated with an increased risk of breast cancer, likely due to higher lifetime estrogen levels, which influence both bone strength and breast cancer development.
- Estrogen Connection: Women with high estrogen exposure throughout life (e.g., early menstruation, late menopause) tend to have higher bone density and are also at a slightly elevated risk for breast cancer.
- Impact of Breast Cancer Treatments on Bone Health
- Chemotherapy & Bone Loss: Some breast cancer treatments, including chemotherapy and ovarian suppression therapy, can induce early menopause, leading to bone loss and an increased risk of osteoporosis.
- Hormonal Therapies (e.g., Tamoxifen & Aromatase Inhibitors):
- Tamoxifen (for premenopausal women) may help preserve bone density but has its own risks.
- Aromatase inhibitors (for postmenopausal women) significantly reduce estrogen levels, increasing the risk of osteoporosis and fractures.
- Corticosteroid Use: Some cancer patients are prescribed steroids to manage side effects, which can also contribute to bone weakening.
- The Need for Dual Screening
- Women undergoing breast cancer treatment should have regular bone density exams (DXA scans) to monitor osteoporosis risk and take preventive measures such as:
- Calcium and vitamin D supplementation
- Weight-bearing exercises
- Medications to prevent bone loss (e.g., bisphosphonates or denosumab)
Mammography and bone density scans play complementary roles in breast cancer management:
- Mammography detects breast cancer early.
- Bone density exams help monitor the effects of treatment and guide strategies to maintain bone health in breast cancer survivors.
Women diagnosed with breast cancer or undergoing long-term hormone therapy should combine both screenings to ensure comprehensive care and minimize health risks.
Causes and Effects
-
Causes: Breast cancer development is influenced by genetic, hormonal, and environmental factors. Risk factors include age, family history, certain genetic mutations (e.g., BRCA1/BRCA2), and prolonged estrogen exposure. Osteoporosis, characterized by decreased bone density, can be exacerbated by breast cancer treatments like chemotherapy and hormone therapy, which may induce early menopause and reduce estrogen levels, leading to bone loss.
-
Effects: Early-stage breast cancer may not present noticeable symptoms, underscoring the importance of regular screenings. Advanced stages can lead to lumps, breast pain, and changes in breast appearance. Osteoporosis increases the risk of fractures, impacting mobility and quality of life.
Solutions
-
Screening and Early Detection: Regular mammograms are essential for early breast cancer detection, improving treatment outcomes. Women should discuss personalized screening schedules with their healthcare providers.
-
Bone Health Management: Patients undergoing breast cancer treatment should monitor bone density. Preventive measures include adequate calcium and vitamin D intake, weight-bearing exercises, and medications to strengthen bones if necessary.
Statistics
-
Breast Cancer: In 2024, an estimated 310,720 new cases of invasive breast cancer are expected to be diagnosed in U.S. women. The chance that a woman will die from breast cancer is about 1 in 39 (approximately 2.5%).
-
Bone Density and Breast Cancer Risk: Some studies have found that women with higher bone mineral density may have an increased risk of developing breast cancer, suggesting that BMD could be considered a biomarker for breast cancer risk.
Analysis: Strengths and Threats
Strengths:
-
Early Detection: Mammography can identify breast cancer before symptoms arise, significantly improving survival rates.
-
Increased Awareness: Public health campaigns have heightened awareness, leading to more women participating in regular screenings.
-
Bone Health Monitoring: Bone density exams facilitate the early detection and management of osteoporosis, particularly important for breast cancer patients on treatments affecting bone health.
Threats:
-
False Negatives: Mammograms may miss some cancers, especially in women with dense breast tissue, potentially delaying diagnosis.
-
Overdiagnosis: Screening might detect cancers that would not have caused harm, leading to unnecessary treatments.
-
Treatment-Induced Bone Loss: Breast cancer therapies can lead to decreased bone density, increasing fracture risk.
Balancing the benefits of early detection with the potential risks of overdiagnosis and treatment side effects is crucial. Personalized medical advice and informed decision-making are essential for optimal outcomes.

